The post- Covid landscape will be a fertile breeding ground for an increase in chronic stress, anxiety, depression, alcohol dependence and self-harm leading to an overall rise in morbidity, and the number of disability- adjusted life years linked to mental health.
As the COVID-19 continues to take lives across the world, there is another public health crisis that’s showing its ugly head. This new danger will perhaps manifest more death and despair than the corona virus itself.
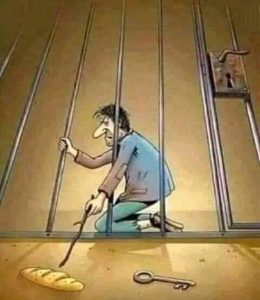
Going by the history of pandemics and an inevitable economic downturn, India is looking at a mental health crisis, with suicide related deaths as its lead indicator.
The social and economic fissures exposed by the pandemic will result in mass unemployment, starvation, homelessness, alcoholism, loan defaults and millions slipping into poverty. At-risk population include 150 million with pre-existing mental health issues, COVID-19 survivors, frontline medical workers, young people, differently abled people, workers in the unorganised sector and the elderly.
For a country with the highest number of poor and malnourished individuals with depression and anxiety this is the ultimate situation. How many suicides can we expect? India reported 1,34,516 suicides in 2018, independent estimates are far more! Thus history tells us India should prepare itself mentally for the numbers in 2020.
Interestingly other than human suffering, suicide has an economic dimension as well. Each death costs Rs 265,000 in the first year alone says a study in the Indian Journal of Psychological Medicine. Short-term costs include hospital expenses, autopsy expenses, police investigations, funeral expenses etc. Long-term costs include the lost income that could have been earned by the person till retirement, tax that the government lost from the income among other things.
Practical applications could be:
Firstly India can appoint a minister with a Cabinet rank as head of mental health and well-being and create an emergency task force of public health experts in creating and executing evidence- based interventions.
Secondly to implement the Mental Healthcare Act 2017 (MHCA) that promises mental health care to all and introduce a suicide prevention policy. Many countries including China have been able to significantly reduce suicides after they implemented a suicide prevention policy. India’s investment in mental health – the last Union budget slashed it by 20% from Rs 50 crore to Rs 40 crore will therefore need a boost.
At the centre of all this there should be a large public engagement campaign to increase help-seeking. This must be centrally driven and supported by state governments. Mental health and suicide should be treated as a public health crisis that needs immediate fixing. Mainstream media and social media may be roped in to create awareness. There is also a good chance that alcohol addiction will rise after COVID-19. It will be beneficial to provide rehabilitation services that address both physical and psychological aspects.
To reduce the pressure on the overworked primary and secondary mental health task force, the focus should be on self, family, community and primary care. Group psychological support for the unemployed through non-profits and the community will help. Training in suicide prevention techniques and combining crisis intervention by providing psychological first-aid will help save lives and reduce emotional distress, preventing long-term trauma.Digitally-mediated therapy and tele psychiatry should be scaled up. NIMHANS in Bengaluru runs a successful telepsychiatry intervention. Similar types of these units should be started in other states as well.
Finally every crisis is an opportunity. The 1918 global flu epidemic made many European countries to create national health services. India should too sit up and realise the negative impacts and consequences of ill psychological health. Thus mental health and suicide prevention can not only save lives but also make immense economic sense.












I appreciated the fact that solutions have been suggested. We usually come across similar analyses but with no clear matter of fact answers. I personally didn’t know about the MHCA and feel that the existence of this Act should be advertised or spoken about. The more we all propagate mental health to be an essential part of general health, the better it is. Thanks for indicating that the government must increase its participation in this. Look forward to your next write up!