The Fall-out
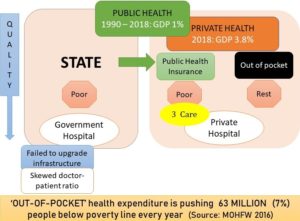
The primary goal of such ‘catch as you can’ mode of private practice ensures maximum profit for either big capital (i.e. corporate hospital) or small capital (i.e. nursing home), extracted out of the exploitation of skilled (doctors and nurses) labor force. This in turn gives rise to rapacious individualism within doctors themselves who tend to benefit at the expense of the miseries of fellow man. Overall, the rich tends to benefit from such exclusive ‘quality’ treatment. But the rest majority are at the receiving end of suboptimal ‘quality’ of treatment because of such poor infrastructure and untrained doctors and nurses, within the scarcity of government hospitals and health centres resources. This had led to three unintended outcomes over the last 30 years:
- People are forced to incur ‘out of pocket’ expenses in private sector which is forcing 63 million patients below poverty line every year. The State sponsored insurance schemes like Ayushman Bharat and Sasthya Sathi, etc. which covers inpatient tertiary care expenses in private sector have failed to reverse this trend because about 85.9% of such ‘out of pocket’ expenses are caused by ‘over the counter’ medicinal purchases, laboratory investigations, etc. i.e. mostly taking place within the ambits of primary care and not covered under any insurance schemes. The health policy plan, 2015 in fact reported that provision of drugs which account for 52% of the total ‘out of pocket’ expenses are not covered, while conditions falling under such insurance schemes cover less than 10% of mortalities, and 15% of morbidities, leaving behind over 75% of communicable diseases uncovered.
Meanwhile, the State budgetary allocations for health sector continue to stagnate at around 1% of GDP for the last 30 years. [1] India ranks 184 out of 191 countries in terms of % of GDP spending on health which stands at around $29 (considering purchasing power parity). Sri Lanka, China, Thailand in fact all invest 3-4 times more per capita. That means the already scarce State revenues are getting diverted further into the hands of the insurance sector and big corporate hospitals, at the expense of public health resources. Ayushman Bharat is the perfect example which has an annual budgetary allocation of Rs 12,000 crore. This is while, the ‘health and wellness clinics’ which are just the extension of existing SCs and PHCs are allotted just Rs 1,500 crore i.e. Rs 1.5 lakh per centre for upgradation.
- Other than such economic fall-out, India has earned the distinction of having one of the worst health indices in the world. Global Disease Burden Study 2015’ published its much-anticipated Healthcare Access Quality (HAQ) Index which compared healthcare access and quality amongst 195 nations from 1990 to 2015. It was based on death rates for 32 diseases that can be avoided or effectively treated with proper medical care. India here stood at dismal 154 (out of 195 counties) with a score of 44.8, just better of Afghanistan and Pakistan. This economic powerhouse shamefully lags behind countries like Sri Lanka which is ranked as high as 73, followed by China (Ranked 82), Bangladesh, Bhutan, and Nepal. The criticism goes beyond numbers as the Lancet goes on to comment that ‘New-born in war ravaged Somalia and Afghanistan has a better chance of survival than in India’. To make matters worse, every third malnourished child in the world comes from India. This provides the perfect milieu for communicable diseases like tuberculosis to flourish.
The lame official excuse propagated by paid-media to justify State helplessness citing ‘huge population burden’ and ‘world economic crises’ has come for serious introspection as the study also published frontier HAQ index which calculates the ‘potential’ health care access and quality based on the Social Development Index (SDI). SDI is a measure of overall development consisting of income per capita, average years of education, and total fertility rates. Thus, frontier HAQ index allows us to quantify the maximum levels of health-care access and quality which can be achieved across the development spectrum of that particular country, and pinpoint geographies where gaps between observed and potential levels have narrowed or widened over time. Several countries, particularly in eastern and western sub-Saharan Africa, reached HAQ Index values similar to or beyond their development levels, whereas others, namely in southern sub-Saharan Africa, the Middle East, and south Asia, lagged behind what geographies of similar development attained between 1990 and 2015. India is amongst the worst offenders, falling behind the expected health standards miserably. India today is home to 21% of world’s disease burden, world’s highest number of women dying in childbirth, and world’s highest number of deaths under the age of five. This comes with no surprise considering that we have the world’s tiniest health budget.
- Doctors are the most recent victims of this fallacious ‘out of pocket’ healthcare system. Earlier, the common man who could not afford quality treatment would just curse his fate. But with time, this frustration and anger had started to pile up. The political class was quick to intervene as they colluded with the media and started a malicious propaganda against doctors to cover up their fallacies. Doctors are most vulnerable entity in this healthcare system as they stand between life and death and become easy victim of all these frustration and anger. On the other hand, some doctors have over the years have given into unethical practice, coaxed by easy money promoted by private business interests. This exploitation of ignorance of a common man is now highlighted by the political class to divert the attention from them. The private healthcare system which promotes such unethical practice is equally to be blamed. But it remains unscathed, thanks to the business interests of the ruling class. In reality, commodification of health care and subsequent deterioration of people’s health is intricately related to violence against doctors and until and unless this is addressed, violence against doctors will not stop.
[1] WHO data, 2019