[First published in Historia Hospitalium, ed. Gunnra Stollber, Christina Vanja and Ernst Krass (Hg.), Band 29, 2021-2013, pp. 45-74. Published by Lit Verlag, Berlin]
Charaka-Saṃhitā (hereafter CS), one of the earliest medical texts of India, provides description of building a hospital, or “a kind of infirmary”[1]. Chapter fifteen (15.5-7), called upakalpanīya, describes thus: “In the first place a mansion must be constructed under the supervision of an engineer well-conversant with the science of building mansions and houses. It should be spacious and roomy. The element of strength should not be wanting in it. Every part of it should not be exposed to strong winds or breezes. One portion at least should be open to the currents of wind.”[2]
Moreover, there were also provisions for number of men who were “skilled in singing, making music, telling or reciting various kinds of stories in prose and verse (ullāpaka, śloka, gāthā, ākhyāyikā, itihāsa, purāṇa).”[3] “A cow should also be kept, yielding copious milk, of a quiet disposition, healthy, having all her calves living.”[4]
Arguably, in an era of bio-medicalization as well as techno-medicine, the hospital and the experience of the patient does take up an extreme turn completely different from the previous description and experience. It is tellingly described in an important textbook of internal medicine:
The hospital is an intimidating environment for most individual. Hospitalized patients find themselves surrounded by air jets, button, and glaring lights; invaded by tubes and wires; and beset by the numerous members of the health care team – nurses, nurses’ aides, physicians’ assistants, social workers, technologists, physical therapists, medical students, house officers, attending and consulting physicians, and many others. … It is little wonder that patients may lose their sense of reality.[5]
In such a hospital, patients almost cease to be persons, and the person of the patient gets reconstituted to be some conglomerations of pathology inside the body. “Removed from their normal surroundings they can be treated in ways that ignore those surroundings precisely because the physician is now focusing on disease entities.”[6] Risse comments, “As depicted by contemporary narratives, going to hospital resembles a journey to a foreign, exotic land, an often too common pilgrimage in which patients cross into a world of strange rites, miraculous interventions, and frequent death.”[7] Additionally, in this present setting of health care, “discussions about health care delivery have focused on value, defined as health outcomes achieved per dollar spent.”[8] While charting out the history of hospitals, which, as scholars ague, evolved into the phase of hospital medicine, Risse points out that for those who enter the space of hospital have to undergo temporally built normative formal initiations.[9] Rebuilding of hospital space and architecture and reconstruction of the notion of time are two important aspects of the new medicine. It is not merely description of hospitals.
It may be beneficial to have a closer look into the date of CS. Wujastyk places it between third or second centuries BC and the period of Gupta dynasty (320 – 420 AD). The latter date corresponds to the period when CS gets frequently quoted.[10] Meulenbeld on the other hand carefully scrutinizes the philosophical material of CS. “The same material suggests that the author called Caraka cannot have lived later than about A.D. 150-200 and not much earlier than about 100 B.C.”[11] References to a king, certain types of officials, and of hospital, together with signs showing that the central administration of the state was growing weak point to the fact that CS “belongs to the Mauryan empire or the period of Śuṅgas.”[12]
In the narrative of CS, we find the patient in a milieu which actually does not dissociate him from his domestic setting, rather the hospital becomes an extension of home. “Beds and chairs should be provided with a (flower) vase and spittoon, bed well-equipped with carpet, bed sheet and pillow along with supporting pillows; and should be comfortable for attending to lying down …”[13] Needless to say, all these arrangements were meant for a king or wealthy persons of high social standing – rājānaṃ rājamātramanyaṃ. In Meulenbeld’s terse expression, “Chapter fifteen, called upakalpanīya, on the equipment of a physician, describes a kind of infirmary, with its personnel and equipment, suitable to the treatment of persons of high social status with full course of pañcakarman.”[14]
A few issues open up before us. First, the hospital described here does not seem to be a usual one – the receptacle of the sick. It is meant for wealthy people and for a particular medical purpose (pañcakarman). It does not seem to be equivalent to hospitals of the medieval period – East or West. Second, the evolution of the concept of pañcakarman itself is quite intriguing. Zimmermann finds that it might have been originally synonymous with śodhana, as both categories encompassed emetics, purgatives, drastic enemas, and errhines. “However, since bloodletting (the fifth of evacuant therapies) has fallen into disuse, it was removed from the set of Pañcakarman, and replaced by oily enemas.”[15] It may therefore be extrapolated that in the hospital of Caraka it was no surgical procedure, but a medical one. Third, in Caraka’s account, the body is assumed to be a two-dimensional frame through which doṣa-s, dhātu-s and mala-s (three morbific entities or humors), and saps flow. But in a modern hospital perception of the body is unwaveringly three-dimensional – in the depth of which resides the harbor of disease or pathological anatomy. Moreover, modern hospital becomes a space where the body can be brought under the gaze of medicine and controlled therapeutic trials can be conducted over it.
Hospitals in Ancient and Medieval India
“Medicine and healing were integral parts of Buddhist monasticism from its inception.”[16] Zysk contends that the much discussed second rock edict of Aśoka “in no way proves tht hospitals existed in India in the third century B.C., but suggests that the monk healers’ role of extending medical aid to the laity coincided with the spread of Buddhism during Aśoka’s reign.”[17] An inscription from Nagarjunikonda, dating from the third century C.E., suggests that a health house for the care of those suffering and recovering from fever was part of this famous Buddhist monastery.[18] Though there remains confusion regarding the exact meaning of fever. Zysk notes, “When Buddhism was submerged in India after 1200, these Hindu institutions seem to have assumed the responsibility for medical services previously provided by the Buddhist monasteries.”[19] A sixth century C.E. inscription from the Duḍḍavihāra in Gujarat states that the use of medicines and remedies was for all those who are sick, not only for the monks.[20]
In the seventh-century India, there are oft-quoted records of Hiuen Tsiang (A.D. 690). In his description, “in all the highways of the towns and villages throughout India he erected hospices, provided with food and drink, and stationed there physicians, with medicines for travelers and poor persons round about, to be given without any stint.”[21] He also mentions of puṇyaśālā or “a house of merit” or “houses of charity”. “The nobles and householders of this country have founded hospitals within the city, to which the poor of all countries, the destitute, cripples, and the diseased may repair. They receive every kind of requisite help gratuitously. Physicians inspect their diseases, and according to their cases order them food and drink, medicine or decoctions, everything in fact that may contribute to their ease.”[22] Secular matrix of Buddhsit medicine becomes evident throughout this narrative.
It should be remembered that until the twelfth century, in Europe, most hospitals were small and basic and seldom offered medical care. The hospital was a guest house and infirmary in one. The care of the sick poor was a duty incumbent upon Christians from the earliest times. Guthrie wryly comments, “Whatever obstacles the Church may have placed in the path of scientific medicine, there was no hindrance, but rather encouragement, in the provision of housing and nursing for sick and wounded persons.”[23] These early hospitals were refuges for sick poor people who were admitted for shelter and basic nursing care and were also a means of isolating those with infectious diseases.[24] There existed “upwards of 750 such charitable institutions in Mediaeval England.”[25] The story of the birth and evolution of the hospital has even been seen as a record of the conquest of barbarism by civilization and of the triumph of Christian altruism over the selfishness of the pagan ideal.[26]
Somewhat comparable developments are seen in Indian subcontinent too. The provision of medical facilities was made in the Brahminical religious institutions of Northern India during the early medieval period. King Śrīcandra (c. 925-75 A.D.) of South-East Bengal made provision for two physicians, though, to state, not for any hospital. It appears that the people “working in the temple of Brahman received their medical aid from these two physicians.”[27] By this shift in providing medical care, two counteracting issues seem to have arisen. First, medical personnel, much despised by Brahminic culture, begin to be adopted by this culture itself. Second, through this adoption, secular nature of Buddhist medicine begins to crystallize into insulated Branminic tradition.[28] Chakravarti and Ray note, “Prior to c. AD 500, most of our references to physicians and healing-houses are located within urban contexts. The physician appearing in a land grant record is often situated in a rural milieu.”[29]
In his small yet important contribution, Wujastyk has provided a brief of history of hospitals in India, especially in Bengal and South India.[30] Wujastyk specifically talks about his aim:
to bring to the surface and organize important information about hospitals in peninsular South Asia. This preliminary information deserves further study, comparison with related data, philological examination and thoughtful interpretation. We may never get the rich detail of patients’ experiences that fills the pages of Risse’s Mending Bodies, Saving Souls. But we do, at least in the case of Caraka’s Compendium, see into the mind of the physician when he planned his house of healing, and through Vallāla’s Dānasāgara and the Tirumukkūḍdal inscription we gain valuable insights into patronage and funding.
He has also discussed about hospitals of Bengal and Kashmir of twelfth century. Regarding King Vallāla’s hospital, he comments “The hospitals he was proposing to fund were to be substantial (“made of bricks”) and well-equipped and staffed. These institutions seem to be hospitals in a recognizable and formal sense, rather than mere dormitories or religious shelters.”[31] As one would understand, here the primary shift has occurred from religious shrines to an abode of care and healing.
Some interesting facts from Nandipurāṇa (a medieval Hindu religious text) can be referred to here. Though the exact date of the text is difficult to ascertain, it must antedate eleventh century A.D. as “Aparārka (1125 A.D.) quotes a long passage from the Nandipurāṇa about the founding of hospitals (ārogyaśāla) where medicines were supplied free to patients. … The passage further states that a competent physician should be appointed. Hemādri (dāna, pp. 893-95) quotes the same passage and another from the Skandapurāṇa to the same effect.”[32] Chandavarkar finds that Nandipurāṇa extols the philanthropist “whose charities are devoted to the erection of health homes and sanatoria for the benefit of the people.”[33] Mukhopaddhyaya has cited a long passage from Nandipurāṇa:
Good health is a step to the acquirement of religious merit, wealth, pleasure and final emancipation, and so the man who bestows cure to the sick and also he who erects a hospital equipped with good medicaments, dresses, learned doctors, servants and rooms for students, always gain them. The doctor should be well-versed in the religious treatises, experienced, familiar with the actions of medicines, a discriminator of the colour of the roots of the herbals and well-acquainted with the proper season of raising them from the ground, well-trained with the qualities of the juices, (their strength and actions), śāli rice, meat and medicaments, trained in compounding medicines, one who knows well of the physique of men by intelligence, one who knows the temperament and the qualities of the diet, a pathologist who is not idle, well acquainted with the remedial agents for the premonitory signs and sequelae of diseases, proficient in the requirements of time and place, well-read in the medical text-books …
The pious man who erects such a hospital in which the services of good physicians of this nature are retained, becomes celebrated as the virtuous, the successful and the intelligent man in this World. If in such a hospital the kind-hearted man .can cure a single patient of his maladies by simple medicines, oleaginous remedies and compounds of medicinal decoctions, goes to the Brahma’s residence with his seven generations upwards. The rich and the poor acquire religious merit in proportion to the amount of riches they possess; where would the poor man get a hospital and a young physician to cure his diseases? The man secures the eternal regions mentioned before by rendering the sick healthy by the use of roots to some and by good rubbing (with external applications) to others. He who cures the sick suffering from an increase or decrease of the Air, the Bile and the Phlegm by simple remedies, he too goes to such blessed regions (after death) as are secured by those who perform many religious sacrifices (Yajñas).[34]
Chandavarakar’s monograph was published in 1912, followed by Mukhopaddhyaya’s in 1913. So it can be reasonably deduced that the text of Nandipurāṇa was extant at least till the first quarter of the last century. The text is now lost. Aparārka is also cited by Hoernle for “the recensions of non-medical version of Ātreya”.[35] It should be apparent that Aparārka, belonging to the twelfth century, was a person with medical understanding. So it is no wonder if he quotes a long passage from the Nandipurāṇa. Caveat may still remain if we look at the two dates of Chandavarakar and Mukhopaddhyaya. This was the period of the nationalist construction of the history of science. As pointed out by Chakrabarti in case of Hindu Chemistry, “the history of science only had a political and historical value for Ray; it could never become the epistemological tool to unravel the problems of modern science.”[36] A closer scrutiny of the material should help us not to be entangled in the tenor of the nationalist project. P. V. Kane is famous for his magnum opus History of Dharmaśāstra which has been referred to. He cites Nandipurāṇa (Pūrvārdha chap 23 verses 12 ff) in another occasion “to give a comparatively but brief description of ekādaśīvrata.”[37] Another eminent scholar R. C. Hazra discussed about Nandipurāṇa.[38] Taking all these facts into consideration it seems cogent to extrapolate that the reference to Nandipurāṇa with regard to hospitals in medieval India is not a unique thing and does not perhaps feed the nationalist construction of history of science.
In his epigraphic studies on South India, Gurumurthy finds that a large number of inscriptions speak of the establishment of dispensaries called as ātulasālai or vaidyasālai. “Most of them seem to have been manned by a local doctor of hereditary nature, for whose maintenance provision of tax-free land offered to the medical man is called in the records as vaidyakkāni or vaidyavṛtti, kāni or vṛtti meaning share of tax-free land.”[39]
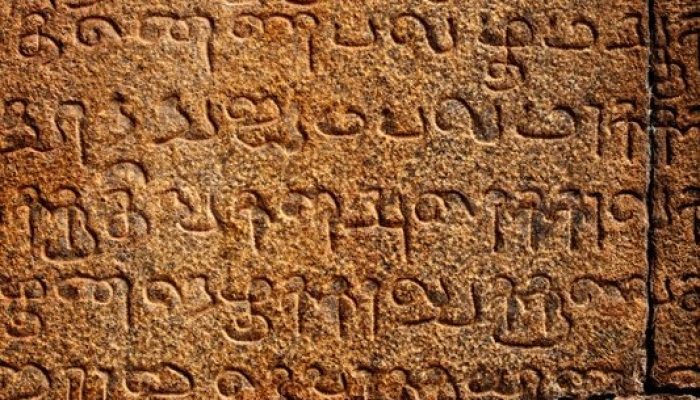
An inscription of the king Vīrājendra, dated in his sixth year (A.D. 1069), is engraved on the east wall of the first prākāra (wall) of the Viṣṇu temple of Veṅkaṭeśa-Perumāl at Tirumukkūḍal in the Madhurantakam taluk (area) of the Chingleput district. The inscription consists of 55 lines of writing and is engraved in two sections. The first section runs to distance of 55 feet. The entire space covered by the inscription is 540 square feet. The language characters of the inscription belong to the latter half of the eleventh century A.D. There were different types of allocations for maintaining different establishments. The last item of expenditure was for the maintenance of a hospital wherein were treated students living in the hostel, and temple servants that were sick.[40] A clear distinction between a physician (Savarṇan Kodaṇḍarāman Aśvatthāma-Bhaṭṭan) and a surgeon (Calliyakkiriyai Pannuvā) becomes evident. The hospital had fifteen beds. Twenty different types of medicines were stored in the hospital. Some of the medicines were of animal origin, most were of vegetable origin. One item seems to be mineral in nature.[41] The physician in charge of the hospital was paid annually 90 kalam (old South Indian unit of measuring weight which varied from area to area) of paddy and 8 kāśu (equivalent to 30 grains) in addition to a grant of land. Contrarily, the surgeon of the hospital received 30 kalam of paddy. Two persons for fetching medicinal herbs were paid 60 kalam of paddy and 2 kāśu. A barber who performed minor operations in addition to his professional duties received 15 kalam of paddy.[42]
We must note that the physician was the highest paid, while the surgeon received payment one-third that of the physician, and lower than persons fetching medicinal herbs and equal to that of barbers. If we remember the previous transformation of pañcakarman into an entirely medical practice, stripped out of its surgical content, inferior position of the surgeon in the eleventh century Brahminic temple makes sense to us. It indicates that there was a downhill journey of surgical knowledge and practice in the scholarly tradition of Indian medical practice. Moreover, there were provisions for preserving medicine throughout the year – “An amount of 40 kāśu (is provided) for purchasing … and for 1 padakku of bovine ghee required to be kept under the earth annually for Purāṇasarpi.”[43]
The thirteenth-century king Viśeśvara established a monastery. The third share endowed by him “was granted in favour of three different institutions which were a Prasūti-śālā, an Ārogya-śālā and a Vipra-satra. The reference to a Prasūti-śālā, i.e., maternity or lying-in hospital, in a record of the thirteenth century is very interesting.”[44]
The Srirangam inscription, dated Śaka 1415 (1493 A.D.), registers the gift of two veli land (old South Indian unit) made by Śrīnivāsa alias Śrīraṅgam Garuḍavāhana-bhaṭṭa who repaired and renovated the Ārogya-śālā or hospital.[45] An arogyasala or a healing-house explicitly figures in an inscription from Siyan (Birbhum, West Bengal), dated to the reign of the Pala ruler Nayapala (c. AD 1027-43). This inscription speaks of a large Śiva temple within the precincts of which stood this hospital. “Medical facilities were made available for both the religious community and the people in general; it has been argued that the inscription indicated that the physicians lived close to the sacred shrine.”[46]
Speziale comments, “The development of hospitals is among the contributions that Muslim culture brought to Indian society, where hospitals were not extremely common institutions at the time that Muslims arrived.”[47] Unlike numerous hospitals in the Christian world, as Speziale notes, hospitals in Muslim cities were not “founded or directed by religious in particular”.[48] For example, under Śīr Śāh Sūrī (r. 1540-1545), separate services for Hindus were introduced in caravansaries established along Indian roads and financed by the state.[49] Two Āyurvedic physicians, whose stipends were paid by the government, “worked at the dār al-śifa of the Śāh Wajīh al-Dīn (d. 1589) shrine in Ahmedabad.”[50] During the reign of Muhammad bin Tughluq (reign 1325-52), “there were around 70 hospitals in Delhi, while 1,200 hakims found employment through the state.”[51] From the book Sirat-e-Fiuz Shahi, it appears that Muhammad bin Tughluq “had established mobile as well as fixed hospitals and appointed competent physicians for each of them.”[52] Sultan Mahmud Khalji of Malwa also erected a hospital at Shādiabad (Mandu) in (A.D. 1445).[53] “Many hospitals devoted to the service of the sick were established in the capital and the outlying cities during the reign of Aurangzeb.”[54]
In Bengal, people came to Pandua from all over Hindustan to receive spiritual training under the sage Nur Qutb al-Alam. He maintained a college, hospital and a langar.[55] Ala al-Din Husayn Shah (1493-1519) made land grants to this college and hospital.
The Bahamani king Alā-ud-Dīn Shāh, the eldest son of Ahmed Shāh al-Walī, built a large hospital at Bidar of South India and endowed lands from the income of which medicine, food, and drink were provided for the sick. He also appointed physicians, both Hindu and Muslim, to treat the patients.[56] It is a sign of accommodating different systems of thought in the operation of the state. During the transition period from Buddhism to Brahminism, as we have seen, similar measures were adopted.
Mahomed Quli built a large hospital Dar-us-Shifa sometime around 1595, now used to accommodate the Hyderabad Municipality offices. The building is a square of 175×175 feet. The hospital was meant to serve the people. The medicines and food to the patients were given free. All the leading Hakeems of the Qutb Shahi period worked in this hospital.[57]
It must be unhesitatingly stressed that I am not an expert to talk about hospitals during the Muslim period in India. Interested readers may go through more helpful resources besides the texts cited.[58]
Transition Times: European Hospitals in India
Since most of Asia’s fundamental tools and mathematical conceptions were familiar to Europe before 1500, the Europeans of the sixteenth century and beyond concentrated upon products rather than devices or ideas.[59] 1735 in more than one ways is a watershed in the history of European scientific attitude. One was the publication of Carl Linnaeus’s Systema Naturae (The System of Nature). In this work, the Swedish naturalist laid out a classificatory designed to categorize all plant forms on the planet, known or unknown to Europeans. The other was the launching of Europe’s first major international scientific expedition, a joint effort intended to determine one and for all the exact shape of the earth.[60] In India, at this early colonial moment, the British grouped indigenous medicine with literature and the arts “considering it to be a part of local tradition distinct from universal science.”[61] It is consistent with the evolution of the concept and meaning of science in Europe. Science came into English in C14. It became more generally used, often interchangeably with art. “But from Mc17 certain change became evident. In particular there was the distinction from art.”[62] Calcutta Review commented, “the great mass of the Hindus are apparently now what the Europeans were three centuries before the Christian era.”[63] W. W. Bird noted, “The Natives have an idea that we have gained everything by our superior knowledge … and they want to put themselves as much as they can upon an equality with us.”[64]
Francois Payrard, a seventeenth-century French traveler, found the Portuguese hospital at Goa to be “finest in the world”. In his experience, “Nothing is done until the physician, surgeon, or apothecary has seen them and certifies that they are sick, and of what ailment, that so they be placed in the proper part of the building.”[65] In the hospital “the great care taken of the sick, and the supply of all comforts that can be wished for, whether in regard to doctors, drugs, and appliances for restoring health, the food is given to eat, or the spiritual consolation that is obtainable at any hour.”[66] Physician’s job was clearly defined, but not that of the surgeon. [67]
In India, Calcutta and Madras were the two cities where military establishments focused on hospital practice. There was visible drive for producing native doctors to reduce the burden of the Company’s exchequer.[68] As early as 1707, in Calcutta, hospitals were built “to keep the men in Health.”[69] It was reported, “Having abundance of our Soldiers and Seamen Yearly Sick and this year more particularly our Soldiers, and the Doctors representing to us, that for want of an Hospitall or Covenient Lodging for them is mostly the occasion of their Sickness, and Such a place as the Companys Charterparty Shipping to keep the men in health.”[70] By 1762 the East India Company’s Bengal army employed nineteen native doctors.[71] In January 1764, the Bengal Medical Service was founded. In Madras, similar developments took place. The surgeons were attempting to establish the city as an important site of medical research and treatment. “The hospital had in fact emerged as a valuable training ground for young medical professionals: by 1772, it was training Europeans, Eurasians, and Tamils in allopathic methods of diagnosis and treatment, and the preparation of medicines.”[72] The Madras system was actually lacking the orientation of simultaneous development of dexterity of both surgery and medicine, as demanded by the new medicine. It was content with primarily producing dressers from the half-castes of the army. “But let not these be confounded with the native surgeons who were attached to our army” – was the cautionary note.[73]
In his insightful work, Harrison traces the dissection-based clinical practice in the East India Company’s medical service, which became one of the key factors in the development of hospital medicine in India. In his opinion, “developments within the armed forces prefigured those normally associated with the ‘birth’ of clinico-anatomical medicine at the Paris hospitals in the 1790s.”[74] He also cogently notes that certain other features of “hospital medicine” are also evident in the Company’s service – “systematic bedside observation, the statistical analysis of cases, and the testing of what were presumed to be economical mass remedies.”[75] Focusing on a prerequisite of hospital medicine, he argues, “In Britain, the supply of bodies for dissection was still severely restricted, but there were no such constraints in the colonies, where cadavers were plentiful.”[76] As a result, practitioners working in the colonial hospitals were “able to compare post-mortem findings with the symptoms of disease in living patients, giving rise to a system of medicine not unlike that which later developed in revolutionary Paris.”[77] Along with this, there was the growing awareness that “men had economic value – and the articulation of this in systems of military accounting – provided a powerful stimulus to the improvement of medical provisions in foreign stations and other measures to conserve manpower.”[78] The hospitals of three presidencies – Calcutta, Madras, and Bombay – were “capable of providing the kind of environment that was conducive to medical innovation.”[79]
Hospitals and Hospital Medicine: European Perspective
During the late eighteenth century there emerged epistemological transformations in the understanding of hospital and medicine. Ackerknecht has designated it as “hospital medicine”.[80] To put it summarily, hospitals were for large numbers of sick people to be investigated and treated; doctors examined patients routinely by techniques such as palpation, percussion, and auscultation; necropsy was a routine way of learning about the nature of diseases and explaining clinical findings; diseases were envisaged as lesions of the tissues that could be analyzed experimentally with the hope of eradicating them altogether; statistical studies of patients and clinical trials were undertaken; and doctors were trained in both medicine and surgery and learnt their profession largely by working with established practitioners at the bedside, embodied in clinical teaching.[81]
With institutional cross-infections and persistent high mortality, these hospitals provided the necessary human tools for advances in clinical medicine and pathological anatomy. Risse argues, “In the controlled ward environments, substantial numbers of inmates, alive and dead, were selected for systematic study, classification, and dissection. Most remarkable were the implications of accurately mapping the sick body with the new techniques of physical examination.”[82] A newly conceptualized medicine started at death, when the bedside-practitioner gave up and the scientist-practitioner took over – and these were the same person.[83] With the rise of hospital medicine it was no longer possible to practice without examination. “Surgeons, used to extirpating the lesions of the disease, and physicians, used to administering systemic medicaments, all suddenly now needed a blanket system that could unite heretofore disparate perspectives on the ‘seats and causes of disease’.”[84] To this day, this method of bedside teaching at hospitals – previously noted in Edinburgh and Vienna – has remained one of the central aspects of medical education. New in Paris, however, was the strategy of total immersion in hospital life – reflected in management routines with long and exhausting hours of work – that similarly survive as a rite of passage for professional and later specialty certification.[85] Every time the new diagnostic technique like stethoscope was (and is) applied to a patient, it reinforced the fact that the patient possessed an analyzable body with discrete organs and tissues which might harbor a pathological lesion.[86] The new Parisian style of hospital based practice, research, and teaching had a resounding impact on medicine throughout Europe and America.
Indian Scenario: Prelude to Hospital Medicine
W. E. E. Conwell was possibly the first person to submit the cases he studied and his notes on the stethoscope to judgments of his colleagues in India in 1827. In his own words, “By submitting to the Profession generally, detailed statements of pulmonary diseases in India; I fulfil (sic) my promise to that effect, made at the request of my excellent and learned master M. Laennec, of Paris”[87] He had reported 25 autopsies in his book out of which 23 cases were native.
In the late eighteenth-century Madras hospital training, the use of stethoscope (invented by Laennec in 1816) was inconceivable. Following the foundation of the Native Medical Institution (NMI, 1822-1835) in 1822 in Calcutta for the instruction of native students in European medicine through vernacular, this new diagnostic technique became popular among the Company’s surgeons and Indian doctors. John Gilchrist and others opined, “the Madras government had sent a particular class of individuals, the sons of soldiers – a sort of half-castes – to be educated at the hospitals as sub-assistant surgeons.”[88] It was also argued, “As to the Madras establishment, and the way in which the pupils were there instructed, it had not the smallest analogy to the medical school for native doctors. Every regiment had three or four native doctors attached to it.”[89] Instead of Madras half-castes as dressers in a regiment, native doctors acted almost like a European doctor. “In May 1825, the Medical Board submitted a report, explaining the reasons why it appeared inadvisable to adopt the Madras system of employing as doctors those who served as dressers in the hospitals, and also explaining satisfactorily both to the Government and to the Court the superior usefulness and success of the school for native doctors, as it had been established, and was then conducted, in Calcutta.”[90]
For the purpose of acquiring practical knowledge of modern medicine like pharmacy, surgery, and physic, the pupils of NMI were attached to the Presidency General Hospital, the King’s Hospital, the Native Hospital, and the Dispensary. “Eight of the pupils who had been educated in this seminary were appointed native doctors, and sent with the troops serving in Arracan.”[91] It was widely accepted that “the British government could not have established an institution calculated to be of greater benefit … than the Native Medical Institution.”[92] Additionally, though the new kind of secular medicine was in the making, it had to accommodate specific socio-economic, political and military exigencies of the colony, which threatened the secular matrix of modern medicine – “Hindoos and Mussulmans were equally eligible. if respectable; the sons of native doctors in the service to be preferred.”[93]
During the prevalence of cholera in Calcutta in 1825 the pupils of this institution “were most usefully employed distributing medicines in different thanah, stations, and in affording to the wretched and numerous victims of the disease, every assistance in the power of European art to bestow.”[94] Besides ramifying the primordial tentacles of public health in India, NMI did another important job for military service, which became more conspicuous after its abolition, “The body of servants was much needed, as the requisite supply of these subordinates has entirely ceased since the abolition of Dr. Tytler’s Native Medical School, and the demand for their services, in the Native Regiments especially, has become very urgent.”[95] The differentiating feature between NMI and Calcutta Medical College (CMC) was the practice of cadaveric dissection in the latter. Unlike Tytler’s NMI, in CMC “the subjects are taught practically, by the aid of the Dissecting Room, Laboratory, and Hospital.”[96] Besides this, the new techniques of investigations like thermometer and stethoscope and new modes of physical examination like inspection, palpation, percussion and auscultation were introduced in these institutions. Importantly, the brief phase of NMI and medical classes at the Calcutta Sanskrit College was the period of the gestation of hospital medicine in India. It was important in another aspect. “The pupils of the Native Medical Institution…keep a case-book of the symptoms and treatment of the sick on the establishment.”[97] This was for the first time in India that students were inducted in individual case-history taking, which was hitherto unknown to them.
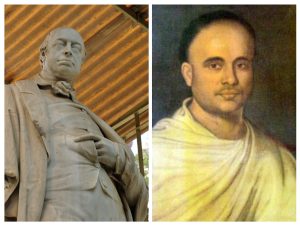
In 1826, Dr. John Tytler, then Superintendent of NMI, began his lecture according to Western method at the Calcutta Sanskrit College on Medicine, and “Professors were appointed to teach Caraka, Suśruta, Bhāva Prakāśa, etc. Classes for the Āyurvedic students were opened in 1827.”[98] Tytler organized his classes around four major departments of medical science, viz Anatomy, Pharmacy, Medicine and Surgery.[99] A medical and an English class had been formed. The report of 1828 stated that the progress of the students of the medical classes had been satisfactory “in the study of medicine and anatomy; and particularly that the students had learned to handle human bones without apparent repugnance, and had assisted in the dissection of other animals.”[100] They also “performed the dissection of the softer parts of animals”, and “opened little abscesses and dressing sores and cuts.”[101] Trevelyan wrote, “The systems of Galen and Hippocrates, and of the Shasters, with the addition of a few scraps of European medical science, was (sic) taught in classes … to the Arabic and Sanskrit colleges at Calcutta.”[102]
Tytler’s training of surgery reminds us of the teachings of Suśruta where preliminary surgical practices were done on soft parts of dead animals or fruits and vegetables. Suśruta’s anatomy, learnt by the Ayurvedic students, was reconstituted into modern anatomical knowledge. Jaggi provides a list of books intended for the students at the Sanskrit medical classes.[103] Earlier, in a letter of 18 August 1824, it was observed, “In proposing the improvement of men’s minds, it is first necessary to secure their conviction that their improvement is desirable.” Apprehension was evident in the observation too, “both the learned and unlearned classes … generally speaking, they continue to hold European literature and science in very slight estimation.” To overcome this obstacle with any good effect it was stressed to qualify the same individuals highly in their own system “as well as ours, in order that they may be as competent to refute error as to impart truth, if we would wish them to exercise any influence upon the minds of their countrymen.” [104]
In Fisher’s memoir, “The report of 1829 states that 300 rupees per month had been assigned for the establishment of a hospital in the vicinity of the college.”[105] Though curricula were in accordance with Sanskrit medical works, a hospital of some kind was thought absolutely necessary for proper medical teaching. “There is now every reason that medical education in India will be improved in a very material degree by this institution.”[106] So, for “affording to the medical pupils ample opportunities of studying diseases in the living subject”, the hospital was established.[107] One graduate, N. K. Gupta, who had been trained as an apothecary, was apparently doing quite well in the position at the hospital. “Though no Hindu had yet performed a major operation, they regularly performed minor ones such as “opening little abscesses and dressing sores and cut”.”[108] Return of the Hospital attached to the Sanskrit College for the year 1832 shows that out 94 House Patients 84 were discharged and six died.[109] Mr. Wilson, who examined the medical class, was ecstatic about “the triumph gained over native prejudices is nowhere more remarkable than in this class”, where “not only are the bones of the human skeleton handled without reluctance, but in some instances dissections of the soft parts of animals performed by the students themselves.”[110] The great end was not to teach any religious learning but useful learning which was gestating the new epistemology of hospital medicine. The English class in the Sanskrit College was eventually abolished in 1835. Interestingly, “this decision was hailed by a section of conservative diehards.”[111] It is understandable that there occurred a change in sign system. The essence of the Sanskrit texts was metonymically reconstituted to suit the purpose of modern medicine. An insidious reconstruction of indigenous cognitive world began its full-fledged operation.
Hooper’s Anatomist’s Vademecum was translated into Sanskrit as Sarira Vidya by Madhusudan Gupta, for which he was paid a sum of 1000 rupees. “It was intended to convey to the medical pandits throughout India, who are an exclusive caste of hereditary monopolists in their profession, and all study their art in Sanskrit, a more correct notion of human Anatomy.”[112] Originally, the Śārīra Vidyā was destined to become a class-book in the medical branch of the Sanskrit College, “but that class had since been abolished, and the teaching of the medical art limited exclusively to English.”[113] The metonymic reconfiguration of indigenous anatomical knowledge into modern anatomical knowledge was too explicit. “Once placed in a Sanskrit dress, the European system of anatomy would be accessible all over India for subsequent transfer into Hindi dialects of every province if requisite, and it was no trivial argument that the same work had been already printed in Arabic, and thus made available for the Musalman practitioners and for translation into Urdu when called for.”[114]
Prior to CMC, NMI and medical classes at the Calcutta Sanskrit College and Madrassa were the conduits through which the new kind of anatomical knowledge could be taught to the students. Before reaching the goal of anatomical dissection preparatory psychological nurturing was done through introduction to zootomy, and handing of bones and skeletons. Owing to my inadequacy, I refrain from discussing Madrassa in this paper.
CMC: The Rise of Hospital Medicine in India
By an order of January 28 1835, the Medical College, Bengal was established. The original order had 34 clauses. Since its inception, under the guidance of Dr. M. J. Bramley, the first principal of CMC, there appears a visible trend in the activities of CMC to introduce basic sciences to its students. During the second year, 1836-37, courses taught at the college were – (a) Practice of Physic by Dr. Goodeve, (b) Elements of Surgery by Dr. Eggerton, (c) Chemistry and Pharmacy by Dr. W. B. O’Shaughnessy, and (d) Introduction to Botany by Dr. Wallich. Third year’s study (1837-38) comprised (a) Anatomy and Physiology by Dr. Gooedeve, (b) Demonstrations and Dissections by Dr. R. O’Shaughnessy, (c) Natural Philosophy and Steam Engine by Dr. W. B. O’Shaughnessy, (d) Structural Botany by Dr. Wallich, (e) Operative Surgery by Dr. Eggerton, (f) Materia Medica by Dr. W. B. O’Shaughnessy, (g) Practice of Physic by Dr. Gooedeve, (h) Elementary Surgery by Dr. Eggerton, and (i) clinical practice in a small hospital attached to the college.[115] Each candidate attended three courses of anatomy and physiology, to of actual dissection, three of chemistry, one of natural philosophy, two of materia medica, two of general and medical botany, two of practice of physic, two of the principles of and practice of surgery and one of operative surgery. In CMC, the most eminent medical officers in the Indian Medical Service were placed in the professors’ chairs. A library, dissecting rooms and a museum were established. “Efforts were made to procure every appliance necessary to place it on the same footing of efficiency as European colleges was (sic) furnished with a bountiful hand.”[116] The twelfth annual report CMC, for the session 1847-48, stated, “There is no institution, connected with the physical or material welfare of the people of this land, whose success we have viewed with more unfeigned satisfaction, than the Medical College of Bengal.”[117]
At its initial phase, CMC had created a space for the nurturance of original, theoretical, and innovative scientific thinking. Unfortunately, it did not germinate. At a time when a chemical laboratory in an American medical school was rare, O’Shaughnessy started his chemistry and botany courses with lectures and “laboratory work was the equal of any in a European medical institution.”[118] Gorman notes, “Most importantly, the students were just as capable and enthusiastic about chemistry as they were about anatomy, and the testimony of outside examiners gives ample proof as to the rigor of the examinations.”[119] O’Shaughnessy proposed to construct, at CMC, a galvanic battery of one thousand cups, on Mullin’s principle “for the purpose of exhibiting the extraordinary experiments recently described by Mr. Crosse and others, and for carrying original researches in electro-magnetism and galvanism.”[120] He even undertook to conduct the “application of galvanism” in case of aneurism.[121] He was also a pioneer of intravenous fluid transfusion for cholera patients.[122] In Calcutta, Dr. Duncan Stewart half-heartedly tried it for cholera patients, but without any results.[123] Bramley’s premature death as well as O’Shaughnessy’s dissociation with CMC seems to put an end to such initiatives at CMC.
In 1839, 70 patients, both European and Indian, suffering from medical and surgical diseases were under treatment at CMC, and the outdoor dispensary attended to 200 patients daily. A few years later, Dr. Mackinnon commented, “Post Mortem examinations were performed by each of the students in my presence and they wrote descriptions of the result” in which “they all evinced practical knowledge … and an acquaintance with the healthy and morbid appearances of the different structures and organs.”[124]
This knowledge was well expressed in a case when “Rumnarain Doss, a student of the Medical College” saved the life of a native youth “who had, by fall, received a severe concussion of the brain.”[125] In 1845, CMC made a great advance, in remodeling its system of instruction “so as to bring it within the regulations of the Royal College of Surgeons in England, and of the Apothecaries Society of London’ so that ‘the Institution may be duly registered and recognized’ in England.”[126]
Notably, within a few months of the discovery of chloroform in 1847 “ether and chloroform” were applied in surgery in CMC.[127] As a result, it was remarkable that among the prominent points of interest were “the extraordinary success among the graduates of the College in the performance of the formidable operation of lithotomy, and the valuable results which had followed the introduction of chloroform into the practice of surgery.”[128] The graduates coming out of CMC served four important purposes. First, it reduced economic expenditure of the Company as “appointing a Sub-Assistant Surgeon to each Native regiment will cost 1,02,000 Rupees a year, whilst their recommendation of a third Native Doctor, will only cost 25,500 Rupees a year.”[129] Second, specifically, their knowledge of stethoscope, microscope and pathological anatomy made them at par with European surgeons. Third, their example set the stage for a veritable flood of Indian students to England for study in all fields, a movement which continues to this day. “The British had invaded and conquered India politically and geographically, but now the Indians had done so in England academically.”[130] Fourth, it met the “wants of the whole northern India by supplying sub-assistant surgeons and native doctors for civil duties and by training medical subordinates for the army.”[131]
- H. Sykes provided reports of 94, 618 patients who were relieved in the Charitable Dispensaries of India in 1847.[132] All these facts make us believe that CMC and its extension through dispensaries into all the corners of Indian society increasingly provided medical and surgical benefit to the people. Initial resistance to hospitalization began to wane.
It should be mentioned that dispensaries served two important purposes in India. Before the foundation of CMC dispensaries were the space where European surgeries and therapeutic experiments with European medicine could be tried. F. H. Brett gave descriptions of “surgical operations performed for expiration of tumours from various parts of the body, removing the cancer and other malignant morbid parts, tying arteries, cutting the stone…”[133] “The advantages of hospital over a Dispensary”, according to him, lay in the fact that in hospital the patient “is never lost sight of by his Medical attendant”.[134] Moreover, in dispensaries disease could not be watched. He employed “Bazaar Medicine” for both economy and watching responses in the patient’s body. After the foundation of CMC, it became a powerful tool to extend the tentacles of hospital medicine, and, thereby, public health in India. Though, to say, dissents against dispensaries were felt within a section of Bengali society as late as 1890.[135]
The foundation of CMC and its subsequent developments became a tool for rewriting a new history of India too – “the seeds of knowledge we have thus sown fructify to a general and luxuriant harvest, that we shall have left a monument with which those of Ashoka, Chundra Goopta, or Shah Jehan, or any Indian potentate sink into insignificance; and their names will fall on men’s ear unheeded, while those of Auckland, as protector, and of Goodeve, Mouat, and others, as zealous promoter of scientific Native medical education shall remain embalmed in the memory of a grateful Indian posterity.”[136] In the ladder of civilization Calcutta came closer to London as hundreds of dead bodies “are daily dissected in London and Calcutta, and new discoveries are being made … bodies are dissected and practical anatomy taught to the pupils…’’[137] Through the production of generations of students and reaching out to population at large, CMC etched out its indelible existence on Indian society. Importantly, unlike Europe, it did not arise out of historical developments in Indian society, rather implanted on India. The traditional practice of Āyurvedics “was challenged with introduction of modern anatomy and medicine … Rather than raise the standards of Āyurvedic practice, these institutions (modern Āyurvedic institutions) reduced the Kavirāja to a simple medicine-man who lacked specialized knowledge of either Āyurveda or allopathy.”[138]
Insightfully, Arnold summarizes the question, “Well into the 19th century, the impact of western medical ideas and practices on India was relatively slight, mostly confined to the larger cities and to the enclaves of the white community and the army. Political and financial considerations weighed heavily against any sustained attempt to change this … Western medicine was never so powerful in India as when it shed its colonial identity.”[139]
CMC played its historical role in the entire process. Hospitals, through their epistemological mutation and transformations, ushered in the era of hospital medicine in India, and marginalization of traditional medicine as well.
________________________
[1] G. Jan Meulenbeld, A History of Indian Medical Literature (hereafter HIML), IA (Groningen: Egbert Forsten, 1999), 17.
[2] CS, trans., A. C. Kaviratna and P. Sharma (hereafter Kaviratna), second revised edition, vol. I (Delhi: Sri Satguru Publications, 2006), 113.
[3] Meulenbeld, HIML, IB, 19.
[4] Kaviratna, CS, 114.
[5] Dan L. Longo et al, Harrison’s Principles of Internal Medicine, 18th edn., vol. I (New York, Chicago: McGraw Hill, 2012), 6.
[6] John Henderson, Pergerine Horden and Alessandro Pastore, “Introduction. The World of Hospital: Comparisons and Continuities,” in The Impact of Hospitals, 300–2000, ed. John Henderson, Pergerine Horden and Alessandro Pastore (Oxford: Peter Lang Publishing Group, 2007), 18.
[7] Guenter B. Risse, Mending Bodies, Saving Souls: A History of Hospitals (New York, Oxford: Oxford University Press, 1999), 9.
[8] Gregg S. Meyer et al., “Two Hundred Years of Hospital and Mortality – MGH and Four Eras of Value in Medicine,” New England Journal of Medicine 366 (2012): 2147-49.
[9] Risse, Mending Bodies, 8.
[10] Wujastyk, Roots, 4.
[11] Meulenbeld, HIML, IA, 114.
[12] Ibid., 112.
[13] CS, trans., P. V. Sharma, vol. I (Varanasi: Chaukhamba Orientalia, 2010), 105.
[14] HIML, IA, 17.
[15] Francis Zimmermann, “Terminological Problems in the Process of Editing and Translating Sanskrit Medical Texts,” in Approaches to Traditional Chinese Medical Literature, ed. Paul U. Unschuld (Doerdrecht, Boston: Kluwer Academic Publishers, 1989), 141-151 (149).
[16] Kenneth G. Zysk, Ascetism and Healing in Ancient India: Medicine in the Buddhist Monastery (Delhi: Motilal Banarsidass, 2000), 44.
[17] Ibid.
[18] Ibid.
[19] Zysk, Ascetism, 46.
[20] Zysk, Ascetism, 44.
[21] Si-Yu-Ki: Buddhist Records of the Western World, trans. Samuel Beal, vol. I (London: Trubner & Co., 1884), 214. The text may otherwise be read as “doctor’s medicines” or “physicians and medicines”.
[22] Ibid, lvii.
[23] Douglas Guthrie, A History of Medicine (London: Thomas Nelson & Sons Ltd., 1945), 128.
[24] Hospitals in a changing Europe, ed., Martin McKee and Judith Healy (Buckingham, Philadelphia: Open University Press, 2002).
[25] Rotha Mary Clay, The Mediaeval Hospitals of England (London: Methuen & Co., 1909), xviii.
[26] John Foote, “Hospitals, their origin and evolution,” Popular Science Monthly 29 (1913): 478-491.
[27] D. C. Sircar, Studies in the Religious Life of Ancient and Medieval India (Delhi: Motilal Banarsidass, 1971), 163.
[28] For transformation of the nature of medical profession, see, Debiprasad Chattoapadhyaya, Science and Society in Ancient India (Calcutta: Research India Publications, 1977).
[29] Ranabir Chakravarti and Krishnendu Ray, Healing and Healers Inscribed: Epigraphic Bearing on Healing-Houses in Early India (Kolkata: Institute of Development Studies Kolkata, 2011), 20.
[30] Dominik Wujastyk, “The Nurses should be able to Sing and Play Instruments”: The Evidence for Early Hospitals in South Asia, accessed 12 June, 2012, http://univie.academia.edu/DominikWujastyk/Talks,
[31] Ibid, 26.
[32] P. V. Kane, History of Dharmaśāstra, vol. II, part II (Poona: Bhandarkar Oriental Research Institute, 1941), 885.
[33] Narayen Chandavarkar, The Heart of Hinduism (Bombay, Calcutta: Times of India Offices, 1912), 25.
[34] Girindranath Mukhopadhyaya, The Surgical Instruments of the Hindus, with A Comparative Study of the Surgical Instruments of the Greek, Roman, Arab and the Modern European Surgeons, vol. I (Calcutta: Calcutta University, 1913, 52-54.
[35] A. F. Rudolf Hoernle, Studies in the Medicine of Ancient India (New Delhi: Concept Publishing Company, 1994), 46, 197-200.
[36] Pratik Chakrabarti, “Science, nationalism, and colonial contestations: P. C. Ray and his Hindu Chemistry,” Indian Economic and Social History Review 37 (2000): 212.
[37] Kane, Dharmaśāstra, vol. 5, pt. 1, 1st edn., 104.
[38] R. C. Hazra, “The Nandi-Purāṇa,” Journal of Ganganath Jha Research Institute 2 (1944-1945): 305-320.
[39] S. Gurumurthy, “Medical Science and Dispensaries in Ancient South India as Gleaned from Epigraphy,” Indian Journal of History of Science 5 (1970): 76-79 (77).
[40] K. V. Subrahmanya Ayaar, “The Tirumukkudal Inscription of Virarajendra,” Epigraphia Indica XXI (1931-32): 220-250.
[41] Ibid, 224.
[42] Ibid, 223-224.
[43] Ibid, 250.
[44] Sircar, Studies, 159.
[45] Ibid, 162.
[46] Chakravarti and Ray, Healing and Healers, 21.
[47] Fabrizio Speziale, “Introduction,” in Hospitals in Iran and India, 1500-1950s ed. Fabrizio Speziale (Leiden: Brill, 2012), 2.
[48] Ibid, 3.
[49] Ibid, 8.
[50] Ibid.
[51] Claudia Liebeskind, “Unani Medicine of the Subcontinent,” in Oriental Medicine: An Illustrated Guide the Asian Arts of Healing, eds., Jan Van Alphen and Anthony Aris (Chicago, IL: Serindia Publications, 1995), 50.
[52] R. L. Verma, “The Growth of Greco-Arabian Medicine in Medieval India,” Indian Journal of History of Science 5.2 (1970): 351.
[53] Ibid, 352.
[54] Ibid, 359.
[55] A. K. M Yaqub Ali, Some Aspects of the Society and Culture of the Varendra, 1200-1576 A.D. (Rajshahi: Rajshahi Univesity, 1998), 180.
[56] Ghulam Yazdani, Bidar: Its History and Monuments (Oxford: Oxford University Press, 1944), 130.
[57] Varja Bolar, “The Role of Islam in Karnataka,” International Journal of Social Sciences and Humanity Studies 3 (2011): 489-498. Also see, D.V. Subba Reddy, “Dar-us-Shifa Built by Sultan Muhammad Quli: The First Unani Teaching Hospital in Deccan,” Indian Journal of History of Medicine II (1957): 102–05.
[58] S. Ali Nadeem Rezavi, “Physicians as Professionals in Medieval India,” in Disease and Medicine in India: A Historical Overview, ed. Deepak Kumar (Delhi: Tulika, 2001), 40-65; O. P. Jaggi, Medicine in India: Modern Period (Delhi: Oxford University Press, 2011), 70-85.
[59] Donald F. Lach, Asia in the Making of Europe, vol. I (Chicago: University of Chicago Press, 1994), 444.
[60] Mary Louise Pratt, Imperial Eyes: Travel Writing and Transculturation (London, New York: Routledge, 1992).
[61] Richard S. Weiss, Recipes for Immortality: Medicine, Religion, and Community in South India (Oxford: Oxford University Press, 2009), 22.
[62] Raymond Williams, Keywords: A vocabulary of culture and society (New York: Oxford University Press, 1983), 277.
[63] “Hindu Medicine and Medical Education,” Calcutta Review xlii (1866): 106-125 (111).
[64] Reports from Committees: Thirty-Two Volumes – East India. Lord’s Second Paper, Vol. XXXII (1852-52), 248.
[65] The Voyage of Francois Payrard, trans., Albert Gray, vol. II, pt. I (London: Hakluyt Society, 1888), 3.
[66] Ibid, 5.
[67] Ibid, 9.
[68] Jayanta Bhattacharya, “Encounter in Anatomical Knowledge: East and West,” Indian Journal of History of Science 43.2 (2008): 163-209.
[69] C. R. Wilson, ed., Old Fort William in Bengal, vol. I (London: John Murray, 1906), 68.
[70] Ibid.
[71] Charles Leslie, “The Professionalization of Ayurvedic and Unani Mediicne,” in Medical Professionals and the Organization of Knowledge, ed. Eliot Freidson and Judith Lorber (New Brunswick, NJ: Transaction Publishers, 2009), 39-54.
[72] Pratik Chakrabarti, “”Neither of meate nor drinke, ubt what the Doctor alloweth”: Medicine amidst War and Commerce in Eighteenth-Century Madras,” Bulletin of the History of Medicine 80.1 (2006): 1-38 (23-24).
[73] “Education of the Native Doctors,” Asiatic Journal and Monthly Register XXII (July 1826): 111-121 (121).
[74] Mark Harrison, ‘Disease and Medicine in the Armies of British India, 1750-1830: The Treatment of Fevers and the Emergence of Tropical Therapeutics,’ British Military and Naval Medicine, 1600-1830, ed. Geoffrey L. Hudson (Amsterdam, New York: Rodopi, 2007), 87-120 ( 89).
[75] Ibid.
[76] Mark Harrison, Medicine in an Age of Commerce and Empire: Britain and Its Tropical Colonies 1660-1830 (Oxford: Oxford University Press, 2010), 4.
[77] Ibid.
[78] Ibid, 18.
[79] Ibid, 22.
[80] Erwin H. Ackerknecht, Medicine at the Paris Hospital 1794-1848 (Baltimore: Johns Hopkins Press, 1967).
[81] John Gabbay, ‘Clinical medicine in revolution: 1 – New elements in the old regime,” British Medical Journal 299 (1989): 106-109. Also see, Ann La Berge and Caroline Hannaway, ed. Constructing Paris Medicine (Amsterdam, Atlanta, GA: Rodopi, 1999).
[82]. Risse, Mending Bodies, 330.
[83] Susan C. Lawrence, Charitable knowledge: hospital pupils and practitioners in eighteenth-century London (Cambridge: Cambridge University Press, 1996), 1.
[84] Charles C. Maulitz, “The pathological tradition,”’ in Companion Encyclopedia of the History of Medicine, eds., W. F. Bynum and Roy Porter (New York, London: Routledge, 1993), 169-191 (178).
[85] Risse, Mending Bodies, 331.
[86] David Armstrong, “Bodies of Knowledge/Knowledge of Bodies,” in Reassessing Foucault: Power, Medicine and the Body, eds. Colin Jones and Roy Porter (London, New York: Routledge, 1994), 17-27.
[87] W. E. E. Conwell, Observations Chiefly on Pulmonary Disease in India and an Essay on the Use of Stethoscope (Malaca: Mission Press, 1829), v.
[88] “Education of the Native Doctors,” 121.
[89] Ibid, 121.
[90] Minutes of Evidence taken before the Select Committee on the Affairs of the East India Company; and also an Appendix and Index. I. Public (16 August 1832), 448.
[91] Ibid.
[92] “Liberality of the Indian Government towards the Native Medical Institution of Bengal,” Oriental Herald and Journal of General Literature X (July-September 1826): 17-25 (24).
[93] Appendix to the Report from the Select Committee of the House of Commons on the Affairs of the East-India Company, 16 August 1832, and Minutes of Evidence. I. Public. (1833), 270.
[94] Ibid, 271.
[95] Report of General Committee of Public Instruction, for the Year 1839-40 (hereafter GCPI), 33.
[96] Ibid, 34.
[97] Original Papers Illustrating the History of the Application of the Roman Alphabet to the Languages of India, ed. Monier Williams (London: Longman, Brown, Green, Longamns, and Roberts, 1859), 57.
[98] Girindranath Mukhopaddhyaya, History of Indian Medicine, vol. 2 (New Delhi: Oriental Books Reprint Corporations, 1974), 15.
[99] S. N. Sen, “The Pioneering Role of Calcutta in Scientific and Technical Education in India,” Indian Journal of History of Science 29 (1994): 41-47 (43).
[100] Minutes of Evidence, 1832, 436.
[101] David Kopf, British Orientalism and the Bengal Renaissance: The Dynamics of Indian Modernization 1773-1835 (Calcutta: Firma K. L. Mukhopaddhyay, 1969), 183-84.
[102] Charles E. Trevelyan, On Education of the People in India (London: Longman, Orme, Brown, Green, & Longmans, 1838), 27.
[103] Jaggi, Medicine in India, 42-44.
[104] Sixth Report from the Select Committee on Indian Territories; together with the Proceedings of the Committee, Minutes of Evidence an Appendix (8 August, 1853), 19.
[105] H. Sharp, Selections from Educational Records, Part I: 1781-1839 (Calcutta, 1920), 183.
[106] Letter, in Public Dept. to Bengal, 24 August 1831, Minutes of Evidence, 1832, 498.
[107] Ibid.
[108] Kopf, British Orientalism, 184.
[109] S. N. Sen, Scientific and Technical Education in India, 1781-1900 (New Delhi: Indian National Science Academy, 1991), 148.
[110] Minutes of Evidence, 1832, 494.
[111] A. F. Salahuddin Ahmed, Social Ideas and Social Change in Bengal, 1818-1835 (Leiden: Brill, 1967), 146.
[112] “Proceedings of the Asiatic Society,” Journal of the Asiatic Society 7.2 (1838): 663-669 (663).
[113] Ibid.
[114] Ibid, 664.
[115] Sen, Scientific and Technical Education, pp. 223-24.
[116] John Clark Marshman, The History of India from the Earliest Period to the Close of the Lord Dalhousie’s Administration, Vol. III (London: Longmans, Green, Readers & Dyer, 1869), 68.
[117] “Annual Report of the Medical College of Bengal. Twelfth year. Session 1846-47,” Calcutta Review 7 (January-June 1847): xliii-xlix (xliii).
[118] Mel Gorman, “Introduction of Western Science into Colonial India: Role of the Calcutta Medical College,” Proceedings of the American Philosophical Society 132.3 (1988): 276-298 (287).
[119] Ibid. p. 287.
[120] “Medical and Physical Society (October)”, Journal of the Asiatic Society and Monthly Register 24 (1837): 64.
[121] O’Bryen Bellingham, Observations on Aneurism, and Its Treatment by Compression (London: John Churchill, 1847), 101.
[122] W. B. O’Shaughnessy, “Proposal of a Kind of Treating the Blue Epidemic Cholera by the Injection of Highly-Oxygenated Salts into the Venous System,” Lancet 17 (1837): 366-371.
[123] “Proceedings of a Meeting of the Medical and Physical Society of Calcutta, 2nd July,” Calcutta Monthly Journal July-December (1836): 313-14.
[124] General Report on Public Instruction, 1852-1855 (1855), 96. Hereafter GRPI.
[125] Calcutta Monthly Journal LII (1839): 171.
[126] “Annual Report of the Medical College of Bengal; Session, 1844-45,” Calcutta Review 3 (1845): xxxiii-xlvi (xxxv).
[127] GRPI, 1847-48, Appendix E, No. VII, cli.
[128] GRPI, 1851, 122.
[129] GRPI, 1847-48, 90.
[130] Gorman, “Introduction of Western Science,” 290.
[131] Annual Report of the Administration of the Bengal Presidency for 1867-68, 121.
[132] W. H. Sykes, “Statistics of the Government Charitable Dispensaries of India, Chiefly in the Bengal and North-Western Provinces,” Journal of the Statistical Society of London 10 (1847): 1-37.
[133] General Committee of the Fever Hospital and Municipal Improvements, Appendices D-F, vol. 7 (Calcutta: Bengal Military Orphan Press, 1838), 205. [West Bengal State Archives]
[134] Ibid, 206.
[135] Anonymous, “Bharate Datavya Cikitsalaya,” Cikitsak 1 (1890, Bengali era 1297): 153-157.
[136] Sykes, “Government Charitable Dispensaries,” 23.
[137] GRPI, 1847-48, Appendix, i-cii (lxxviii).
[138] Brahmnanda Gupta, “Indigenous Medicine in Nineteenth- and Twentieth-Century Bengal,” in Asian Medical Systems: A Comparative Study (Delhi: Motilal Banarsidass, 1998), 375-376.
[139] David Arnold, “The rise of western medicine in India,” Lancet 348 (1996): 1075-78 (1078).